This post will be a little self-indulgent, in that it has been coming for a long time – fifteen months in the making – and that the circumstances surrounding the doxxing, defamation and vilification of a complete stranger, by anti-vaccination activists, continues to this day.
Directly related to the above is another subject which pertains to the alleged illegal sharing of my personal mobile phone number to anti-vaccination activists, I argue, originating out of Holdsworth House Medical Practice (HHMP), in Sydney. Whether or not HHMP knows that they are the source of the alleged illegal sharing of my phone number is up for debate. Below, I will include HHMP’s response to an investigation by the NSW Health Care Complaints Commission (HCCC), regarding a complaint that was lodged about the alleged illegal sharing of my personal information by this healthcare provider. HHMP has not and has never assisted me with any requests I have made of them in this matter.
I will also include responses from the investigating police station at the time, which would appear to be in conflict with the claims made by HHMP to the HCCC. I argue that this is enough to have the HCCC take another look at the claims made by HHMP and, in particular, its staff.
So…
My name is Peter Tierney. I live on the New South Wales South Coast. I am not a healthcare practitioner. I am single. I am a full-time, single parent to my two kids. You can hear my voice in this ABC North Coast interview about this exact topic. This exact topic exemplifies best why I keep my identity – apart from my name – and those of my children, a secret. Check out my testimonials page for further examples as to why this secrecy is a good idea.
My name is not Peter Tiernan. Peter Tiernan lives on the NSW North Coast. He is a healthcare practitioner (a physiotherapist). He is married. As far as I know he has one daughter. You can hear his voice in this ABC North Coast interview about this exact topic, given the day before my interview.
In the course of investigations into this whole debacle, NSW Police verified both of our identities as separate individuals living in different regions of NSW. We both did this in person, at our local police stations, using our real faces and our real driver’s licences with our real names on them.
Anti-vaccination activists, led by Belgin Colak-Arslan and the Australian Vaccination-skeptics Network’s Brett Smith, both of Sydney, wrongly identified Mr Tiernan as me, because: our names are similar; he grew up with the McCaffery family, whom I have known only since 2009; he went to school with journalist Jane Hansen, whom I have only known, but, never met in person, since about 2010; and he is a healthcare practitioner.
Basically, antivaxers put two and two together and got potato. Then they mashed the potato and doxxed Peter Tiernan and his extended family, and continue to defame and vilify Peter Tiernan to this day. They contacted his daughter and his wife on Facebook, for God’s sake. They contacted him at work and threatened him. He had to shut down his social media presence and change his phone number. His work had to start screening his calls due to the threats and abuse. Belgin Arslan even published his address on a public Facebook thread, eliciting a threat from deranged anti-vaccination activist Frank Vazquez:
For greater detail on the doxxing, please read these two articles on the whole doxxing debacle, by Diluted Thinking:
The Doxxing of Peter Tiernan – an Overview
The Doxxing of Peter Tiernan – the Doxxers
So, what tipped these antivax conspiracy theorists over the edge into illegality, apart from their usual Dunning-Kruger certainty?
On October 18 2016, in the course of collecting evidence for my blog series on anti-vaccine nurses and midwives, I came across a Sydney nurse – whom I had noticed some months previously – who bragged in the Anti-Vaccination Australia Facebook group that her workplace knew about and condoned her anti-vaccination activism:
I’m a nurse and will continue to say what I believe about vaccines. They can shove their guidelines up there ass
…my boss and colleagues all know my views on this issue and are fine with it. I have worked here for a long time and my views and beliefs are no secret to anyone in my workplace so I think I’m safe
This nurse was Loretta Blaikie (AKA Loretta Salakas, AKA Loretta Baxter). Blaikie included the name of her employer on her public Facebook profile. Blaikie’s employer is/was Holdsworth House Medical Practice. Exercising due diligence, I called HHMP to verify that she did in fact work there. This was confirmed by the receptionist. I advised the receptionist that I would require Blaikie’s AHPRA registration number – to facilitate a complaint about her anti-vaccination activism that cited her employer’s imprimatur – as Blaikie was not using her AHPRA-searchable, registered names in her antivax activism. The receptionist told me I would need to talk to the nursing unit manager, that the nursing unit manager was unavailable, and that I could leave my name and number for the nursing unit manager. I agreed to leaving my name and number for the stated and specific use of the nursing unit manager only, and for no-one else. I stated that the call was confidential. I received no reply from the nursing unit manager, and so left another message the next morning, October 19 2016, re-stipulating all of the above. Again, I received no reply from the nursing unit manager.
On October 20 2016, at 0819 hours, I published my article on Blaikie: Anti-vaccine nurses and midwives 26.
Blaikie has since had restrictions placed on her registration:
The registrant must not work as an enrolled nurse until reviewed by the Nursing and Midwifery Council of New South Wales and this condition is removed.
A letter sent to complainants, on August 21 2017, by the Nursing and Midwifery Council of NSW, states the following:
Complaint about Ms Loretta Lee Blaikie
Thank you for your letter dated 21 October 2016 about Ms Loretta Lee Blaikie.
The Council considered your complaint and additional information, and decided to take urgent interim action under section 150 of the Health Practitioner Regulation National Law.
Interim conditions have been imposed on Ms Loretta Lee Blaikie’s registration to protect the public. Information about these conditions are available on AHPRA’s website www.ahpra.gov.au. These conditions are temporary and will remain in place until removed, amended by the Council or the complaint is finalised.
On October 20 2016, at 1742 hours, I received a phone call from a senior-constable at a South-Western Sydney police station, who was acting on an in-person complaint of harassment lodged by Loretta Blaikie. I was skeptical that the senior-constable was indeed a police officer due to his thuggish demeanour, his reluctance to provide the phone number for the police station, his vague threats to arrest me, and his devolving argumentation and intimidation which ended in him calling me a “grub.” After some days, verifying with my local police that the call had indeed come from a serving police officer, I lodged a complaint about the officer which resulted in his chief-inspector apologising to me for his behaviour – on November 25 2016 – even though the senior-constable refused to apologise. I agreed to settle my complaint via an informal process. At no stage did I seek disciplinary action. I only ever requested an apology.
While this NSW Police complaint process was ongoing, a friend had lodged a complaint about HHMP to the NSW HCCC – expanded below – regarding the alleged illegal release of my phone number to anti-vaccination activists. A brief account of the fallout of this alleged illegal release of my number – apart from having to change my mobile phone number for valid safety reasons – is as follows.
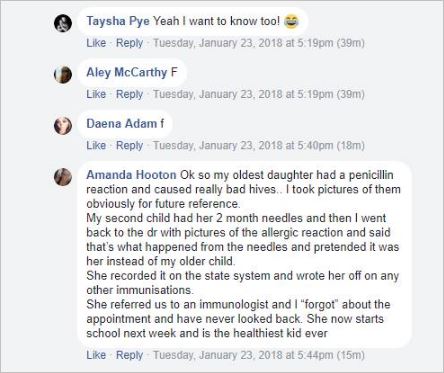
On October 20 2016, at 1833 hours, I received a phone call from anti-vaccination activist Belgin Arslan, on mobile phone number 04******69, who conveyed to me that she had just obtained my private, unlisted phone number from a ‘private messaging thread where my phone number was being shared amongst dozens of anti-vaccination activists’. Arslan refused to state the name of the individual who had started this Facebook messaging thread. On October 22 2016 at 1415 hours, Arslan called me again, this time denying that she obtained my mobile phone number from a private antivax messaging thread. She instead claimed she was given the number by Herald Sun Health Editor Grant MacArthur. Arslan then claimed it was given to her by a female Herald Sun receptionist who gave Arslan my number, after checking through messages which had been left (I had not left any messages with the Herald Sun). Grant MacArthur expressly denied these claims as false and impossible, in an email to me. Colak then begged for her name to be left out of any reports to police on this matter. Colak called and texted me several times throughout the day. She continued attempting to call and text me until the end of October 2016. In an act which speaks volumes to Arslan’s deceit and attempt to cover her tracks, and the tracks of others, she texted me to claim that she and Loretta Blaikie had only become Facebook friends on October 23 2016. I know this is a lie. They had already been Facebook friends for several months when I posted my blog post on Blaikie:
October 20 2016, at 2037 hours, I received a phone call from anti-vaccination activist Brett Smith misrepresenting himself as “Dr Andrew Gowrie” of Holdsworth House, on 04******14. He stated that he was the “on-call doctor”. He stated that he was prompted to call me by, and “on behalf of [his] boss” Dr Dick Quan, Managing Director of HHMP. He stated that he was tasked by Dr Quan to investigate any breaches of privacy at Holdsworth House Medical Practice. On October 21 2016, Smith also sent a text, impersonating Dr Andrew Gowers (a real doctor at HHMP):
October 22 2016 at 1142 hours
I received another phone call from Dr “Andrew Gowrie”. I recognised Brett Smith’s voice on this occasion and searched for a previous message where his number was shared with me. It is the same phone number as this June 16 2016 Facebook message, from Brett Smith:
And it’s also the same number Smith publicly posted to a friend, in 2016, with Smith going on to threaten to assault my friend, over the phone:
When I publicly tweeted that I was now aware of Smith’s impersonation of Dr Andrew Gowers, Smith texted me again:
Smith texted again on October 31 2016, attempting to intimidate me with blog posts:
The threats, intimidation, defamation, and doxxing of Peter Tiernan and me then kicked off, in earnest. This Dropbox collection contains over a dozen PDFs of evidence of this attack on Peter Tiernan and me. Smith published three blog posts based on his and Arslan’s poor investigative skills, all defaming Peter Tiernan, a completely innocent man. These blog posts remain published and Smith retweets them on a regular basis. Given that Smith is aware – even via his own solicitor – that NSW Police have verified that Peter Tiernan is not me, I would argue that Smith’s continued defamation and vilification of Peter Tiernan falls into the category of criminal defamation:
Smith then started implying – with the assistance of Meryl Dorey of the Australian Vaccination-skeptics Network – that we are involved in paedophilia:
Smith has continued his criminal defamation of Peter Tiernan to this day:
Arslan and Smith have also repeatedly boasted of being in the possession of illegally recorded telephone conversations between themselves, me, and Peter Tiernan. In NSW, this is a breach of the NSW Surveillance Devices Act. Both are aware that they did not have permission to record the phone calls, nor share the illegal recordings, nor publish the illegal recordings. To date they have not publicly published these recordings.
Arslan:
November 7 2016
November 12 2016
SURVEILLANCE DEVICES ACT 2007 – SECT 12 Possession of record of private conversation or activity
SURVEILLANCE DEVICES ACT 2007 – SECT 12 Possession of record of private conversation or activity
Finally, we come to Holdsworth House Medical Practice’s response to the NSW Health Care Complaints Commission, in relation to a complaint that HHMP had allegedly, illegally shared my private contact details with anti-vaccination activists. The HCCC findings to the complaint are located here. I will add the full text in an appendix, below.
For now, the pertinent section of the HCCC findings, from December 12 2016, is as follows. I will respond to HHMP’s claims below:
In relation to the allegation the Practice disclosed confidential contact information of Mr Tierney, the Practice advises the receptionist who took his call noted he was not a patient and escalated the inquiry to the Nurse Unit Manager as per his request.
The Practice was advised by Ms Baxter that she had been subject to harassment via a Facebook group and had reported the matter to Police. In turn, Police requested the telephone number of Mr Tierney for the purpose of their report.
The Practice provides statements from staff confirming they did not provide Mr Tierney’s phone number to any party other than the NSW Police at their request following allegations of harassment.
The Practice outline the confidentiality agreements that are signed by all staff members including the receptionist, Nurse Unit Manager and Ms Baxter. It is reiterated that all staff comply with privacy obligations and do not disseminated personal information of patients or otherwise unless consent is provided or they are required by way of subpoena or warrant.
HHMP claimed that an employee gave my phone number to police, on their request:
Police requested the telephone number of Mr Tierney for the purpose of their report.
NSW Police confirmed to me – on November 25 2016 – that the senior-constable to whom Blaikie complained, in person, on October 20 2016, retrieved my phone number from the COPS Database, not from the complainant. The complainant provided my name to the senior-constable. This confirms to me that Blaikie was given my name – and most likely my phone number, by HHMP’s own admission – against my express wishes that this matter was to be treated in confidence, as agreed to by the receptionist.
HHMP again claimed that NSW Police requested my phone number:
The Practice provides statements from staff confirming they did not provide Mr Tierney’s phone number to any party other than the NSW Police at their request following allegations of harassment.
On February 24 2017, NSW Police confirmed to me that the investigating senior-constable “had no recollection” of ever contacting HHMP, and reiterated that he retrieved my number from the COPS Database. So, HHMP provided my number to someone, but, it wasn’t NSW Police.
Again, HHMP stated that NSW Police requested my phone number:
The Practice provides statements from staff confirming they did not provide Mr Tierney’s phone number to any party other than the NSW Police at their request following allegations of harassment.
This is already known to be untrue, per the above. This now demands further explanation from HHMP staff as to whether or not they have lied to the HCCC in their statements, or whether or not they have provided my phone number to anti-vaccination activists impersonating police officers over the phone: this is not a far stretch of the imagination given what antivaxers had already done in impersonating a doctor, and lying about obtaining my phone number from messages left with ‘a female Herald Sun receptionist.’
HHMP admits to staff breaching its own privacy policies and procedures by providing my private details to a third party – who were not the NSW Police – without a “subpoena or warrant”:
The Practice outline the confidentiality agreements that are signed by all staff members including the receptionist, Nurse Unit Manager and Ms Baxter. It is reiterated that all staff comply with privacy obligations and do not disseminated personal information of patients or otherwise unless consent is provided or they are required by way of subpoena or warrant.
Thanks for reading this far.
Hopefully charges will still be laid against Arslan and Smith. There is certainly enough evidence, provided by them.
______________________________
Appendix
HCCC December 12 2016 Holdsworth House Medical Practice findings text
Dear Mr Mcleod,
I am writing to advise you of the Commission’s assessment decision concerning your complaint about Ms Loretta Baxter and also the Holdsworth House Medical Practice Darlinghurst (the Practice).
In order to assess your complaint, the Commission notified the executive of the Practice and requested a response to the issues and allegations you raised. The Practice does not consent to the release of that response to yourself of any third party. As such, I am not lawfully able to supply with you a copy.
The Commission specifically requested the Practice respond to allegations they are anti-vaccination or that they condone promotion of ant-vaccination views within their organisation. Additionally, the Commission sought clarification of the Practice’s policy with regard to anti-vaccination sentiments and activism of their staff, namely Ms Loretta Baxter. Finally, the Commission requested the Practice respond to the allegation their staff released confidential information, that being the personal details of Mr Tierney.
In addition to the response, the Commission considered the volume of Facebook screen captures supplied in your complaint and also received supplementary to your complaint.
In their response, the Practice outlined their involvement in the employment of Ms Baxter, indicating she is employed by Australian Clinical Labs (ACL) who provide pathology and nursing services to the Practice’s central Sydney site. The response states Ms Baxter is an Endorsed Enrolled Nurse who has provided services to the Practice on an intermittent basis for the past 6 years.
The Practice states they strongly promote adherence to vaccination programs across each of their outlets and prior to this occasion, the views of Ms Baxter have never been brought to their attention.
The Commission is advised that over the course of her engagement with the Practice, Ms Baxter has administered hundreds of vaccinations in line with recommended guidance and has demonstrated herself to be an exemplary EEN without any suggestion or feedback she has encouraged patients from being vaccinated.
The Practice states they have reported the views of Ms Baxter to her employer and it is their understanding that she has received formal warning. The Practice advise that whilst the comments of Ms Baxter were made in a Private forum, they have made it expressly clear the conduct of publically expressing such views on vaccination do not accord with the Practice and is unacceptable. They also state publication or further incidents of anti-vaccination sentiments will result in further action which may include termination of her services.
The Commission are advised that Ms Baxter has provided reasoning for her decision not to vaccinate one of her children on medical grounds however she herself is vaccinated as per requirement of her profession.
In relation to the allegation the Practice disclosed confidential contact information of Mr Tierney, the Practice advises the receptionist who took his call noted he was not a patient and escalated the inquiry to the Nurse Unit Manager as per his request.
The Practice was advised by Ms Baxter that she had been subject to harassment via a Facebook group and had reported the matter to Police. In turn, Police requested the telephone number of Mr Tierney for the purpose of their report.
The Practice provides statements from staff confirming they did not provide Mr Tierney’s phone number to any party other than the NSW Police at their request following allegations of harassment.
The Practice outline the confidentiality agreements that are signed by all staff members including the receptionist, Nurse Unit Manager and Ms Baxter. It is reiterated that all staff comply with privacy obligations and do not disseminated personal information of patients or otherwise unless consent is provided or they are required by way of subpoena or warrant.
In conclusion, the Practice undertake their adherence to vaccination programs and offer a spread sheet of demonstrating vaccinations administered. They advise they have issued a formal statement on their Facebook page reassuring consumers of their views on vaccinations and their compliance with privacy laws.
On the 28 November 2016, the Commission Assessment Committee considered all available material and concluded there are insufficient grounds to progress your complaint regarding Holdsworth House Medical Practice.
The Commission determined there is insufficient evidence to indicate the Practice does not adhere to best practice with regard to administration of vaccinations. The Commission concludes that aside from Ms Baxter, there is insufficient evidence to indicate a culture of anti-vaccination activism or sympathies that might pose an ongoing risk to public health or safety or would require further action by the Commission against the facility itself.
The Commission considered the reasoning by the Practice to supply the phone number of Mr Tierney to NSW Police was based on a considered and contained decision and does not draw criticism. You are encouraged to escalate this to the Privacy or Information Commissioner of NSW if you do not agree with this decision as they are the appropriate body to consider complaints about privacy and information.
Whilst the matter did not reach a threshold for further investigation, the Commission makes formal comment to the facility reminding them of their requirement to enforce recognised best science. The Commissioner formally notes the undertakings provided by the executive of the Practice with regard to their vigilance about the views of their staff regarding anti-vaccination and the comments of their staff on social media.
I acknowledge you may have outstanding concerns about the Practice or that you may not agree with the decision of the Commission. However I wish to assure you that the Commission Assessment Committee took this matter very seriously, given the recognised best science regarding vaccination protocols and adherence to practice directives of medical and nursing governance.
Your complaint regarding Ms Loretta Baxter (Blaikie – E. E. N) remains under assessment and is at the stage of co-regulatory consultation with the Nursing and Midwifery Council of New South Wales. The final decision of that assessment may not be available until to the New Year given the Christmas closure period of both the Commission and the Council. This decision will be communicated to you in the first instance and patience is appreciated.
Under our legislation, you are entitled to request a review of the assessment decision. Should you consider that the assessment decision was not thorough and robust, OR if you have any new material for the Commission to consider, you may request a review in writing within 28 days of receiving this letter.
If you have any questions about this decision, please contact…
______________________________